#RTH-AGITATION- Rajasthan – Sadly doctors are fighting for their genuine rights and dignity against all. No one is with them – media, judiciary, Government and not even patients whom they have saved.
Aspiring doctors should know the reality and introspect- why they wish to be a doctors in such circumstances?
Smaller hospital and individual doctors’ clinics are backbone of the health care system in India. Their contribution towards public health can’t be ignored. Be it Covid care or treatment of daily ailments, they are actually helpful to the public and indispensable in real sense. Their contribution to society is huge especially in view of broken public health care system.
They provide health care near to public near their residential area at affordable cost. From an another angle, they generate employment to the workers as well as small businesses associated with their small hospitals.
In a populous country like India, strengthening these smaller hospital is a desirable step. To strengthen the health care, Government can actually do well to support these hospitals and achieve health care to all. Supporting them will require a fraction of resources, as compared to the money needed in case Govt has to provide to public itself.
It will be a short-sightedness of the Government policies, if instead of supporting them, Govt wishes to exploit their resources to give free health care to public.
But administrators and bureaucratic system has failed on both fronts. Neither they were able to develop a dependable health care system for public, nor they tried to support smaller health systems. What they tried to do was akin to the ancient story of ‘ the farmer and the Golden goose’. The Greedy farmer wanted all the golden eggs instantly without feeding the bird and therefore killed the duck. Government with its short-sighted bureaucracy is killing its golden health care and not realizing the real potential and benefits.
In the present day, ebbed from all sides, doctors need to earn back the dignity of profession and resist oppression. The phenomenon of oppression of doctors in the name of regulation is a global issue. The populist oppressive schemes in the misleading names like #RTH-Rajasthan (RIGHT TO HEALTH) are prevalent everywhere globally in some form or another. Doctors and nurses have been reduced to no more than moral and economical slaves either by industry or administrators, not infrequently pulled by legal bridle in their noses.
Will Rajasthan’s Right to health bill do more harm than Good
Acquiring kind of skill , the years of passionate, merciless, excruciating medical learning is placed at the disposal of administrators, who themselves have failed to develop a good health care system in real sense.
#NO-TO-RTH-AGITATION is a movement , the result of failure of Government to create public health system, but it has potential to fail the existing private doctors’ system as well. Smaller hospitals are already on verge of closure, will be forced to shut down. It carries the risk of extinction of neighbourhood friendly doctor and hospitals.
The basic problem is the intentions for the task of developing a good health care system. The agenda of administration is to control the health care workers rather than developing a good health care system for citizens.
What NO-TO-RTH-AGITATION is actually doing? It is a cry for survival of the smaller hospitals- not only for themselves but for Indian Health care system, if short-sighted bureaucracy can understand the real problem.
Advantages-Disadvantage of being a doctor
25 factors- why health care is expensive
21 occupational risks to doctors and nurses
Covid paradox: salary cut for doctors other paid at home
Medical-Consumer protection Act- Pros and Cons
Expensive Medical College seat- Is it worth it?
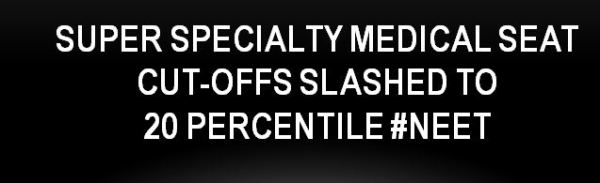
NEET- Not so Neat- percentile system
The Myth of cost of spending on medical education needs to be made transparent.